MONKEYPOX
Monkeypox
• Monkeypox is a viral zoonosis (a virus transmitted to
humans from animals) with symptoms very similar to those seen in the past in smallpox
patients, although it is clinically less severe.
• With the eradication of smallpox in 1980 and
subsequent cessation of smallpox vaccination, monkeypox has emerged as the most
important orthopoxvirus for public health.
• Monkeypox primarily occurs in Central and West
Africa, often in proximity to tropical rainforests and has been increasingly
appearing in urban areas.
• Animal hosts include a range of rodents and
non-human primates.
The Pathogenesis of monkeypox viruses
• Monkeypox virus is an enveloped double-stranded DNA
virus that belongs to the Orthopoxvirus genus of the Poxviridae family.
• There are two distinct genetic clades of the monkeypox
virus – the Central African (Congo Basin)clade and the West African clade.
• The Congo Basin clade has historically caused more severe
disease and was thought to be more
transmissible. The geographical division between the two
clades has so far been in Cameroon - the only country where both virus clades
have been found.
Natural host of monkeypox virus
• Various animal species have been identified as
susceptible to monkeypox virus.
• This includes rope squirrels, tree squirrels, Gambian
pouched rats, dormice, non-human primates and other species.
• Uncertainty remains on the natural history of
monkeypox virus and further studies are needed to identify the exact
reservoir(s) and how virus circulation is maintained in nature.
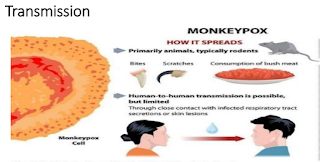
Transmission monkeypox virus
Signs and symptoms
• The incubation period (interval from infection to
onset of symptoms) of monkeypox is usually from 6 to 13 days but can range from 5 to 21 days.
The infection can be divided into two periods:
• the invasion period (lasts between 0-5 days)
characterized by fever, intense headache, lymphadenopathy (swelling of the lymph
nodes), back pain, myalgia (muscle aches) and intense asthenia (lack of
energy). Lymphadenopathy is a distinctive feature of monkeypox compared to
other diseases that may initially appear similar (chickenpox, measles,
smallpox)
Signs and symptoms
2nd phase
• the skin eruption usually begins within 1-3 days of
appearance of fever. The rash tends to be more concentrated on the face and
extremities rather than on the trunk. It affects the face (in
95% of cases), and palms of the hands and soles of the
feet (in 75% of cases). Also affected are oral mucous membranes (in 70% of
cases), genitalia (30%), and conjunctivae (20%), as well as the cornea. The
rash evolves sequentially from macules (lesions with a flat base) to papules
(slightly raised firm lesions), vesicles (lesions filled with clear fluid),
pustules (lesions filled with yellowish fluid), and crusts which dry up and
fall off. The number of lesions varies from a few to several thousand. In severe
cases, lesions can coalesce until large sections of skin slough off.
Course
of Illness
• Monkeypox is usually a self-limited disease with the
symptoms lasting from 2 to 4 weeks.
• Severe cases occur more commonly among children and
are related to the extent of virus exposure,patient health status and nature of
complications.
• Underlying immune deficiencies may lead to worse
outcomes.
• Although vaccination against smallpox was protective
in the past, today persons younger than 40 to 50
years of age (depending on the country) may be more
susceptible to monkeypox due to cessation of smallpox vaccination campaigns
globally after eradication of the disease.
• Complications of monkeypox can include secondary
infections, bronchopneumonia, sepsis, encephalitis, and infection of the cornea
with ensuing loss of vision. The extent to which asymptomatic infection may
occur is unknown.
• The case fatality ratio of monkeypox has
historically ranged from 0 to 11 % in the general population and has been
higher among young children. In recent times, the case fatality ratio has been
around 36%.
Diagnosis of monkeypox
• The clinical differential diagnosis that must be
considered includes other rash illnesses, such as chickenpox, measles,
bacterial skin infections, scabies, syphilis, and medication-associated
allergies.
• Lymphadenopathy during the prodromal stage of
illness can be a clinical feature to distinguish monkeypox from chickenpox or smallpox.
• Polymerase chain reaction (PCR) is the preferred
laboratory test given its accuracy and sensitivity-For this, optimal diagnostic
samples for monkeypox are from skin lesions – the roof or fluid from vesicles
and pustules, and dry crusts. Where feasible, biopsy is an option.
Therapeutics of monkeypox
• Clinical care for monkeypox should be fully
optimized to alleviate symptoms, manage complications and prevent long-term
sequelae.
• Patients should be isolated and offered symptomatic
treatment with fluids and food to maintain adequate nutritional status.
• Secondary bacterial infections should be treated as
indicated.
• An antiviral agent known as Tecovirimat that was developed for smallpox was licensed by the European Medical Association (EMA) for monkeypox in 2022 based on data in animal and human studies. It is not yet widely available.
Vaccination of monkeypox
• Vaccination against smallpox was demonstrated
through several
observational studies to be about 85% effective in
preventing
monkeypox. Thus, prior smallpox vaccination may result
in milder
illness.
• At the present time, the original (first-generation) smallpox vaccines are no longer available to the general public.
• A still newer vaccine based on a modified attenuated vaccinia virus (Ankara strain) was approved for the prevention of monkeypox in 2019. This is a two-dose vaccine for which availability remains limited.
Prevention of monkeypox
• Raising awareness of risk factors and educating people about the measures they can take to reduce exposure to the virus is the main prevention strategy for monkeypox.
• Scientific studies are now underway to assess the
feasibility and appropriateness of vaccination for the prevention and control
of monkeypox.
• Some countries have, or are developing, policies to
offer vaccine to persons who may be at risk such as laboratory personnel, rapid
response teams and health workers.
• Other measures include prevention of Animal-Human
& Human- Human transmission
- CORONA VIRUS
- MONKEY POX
- VAGINAL DRYNESS
- FIBROID
- INFERTILITY
- OVULATION CYCLE
- OVARIAN CANCER
- VAGINAL BACTERIA
- MALE INFERTILITY
- BEST DAYS OF CONCIEVING
- MUCUS AFTER OVULATION
- FOODS FOR ERECTILE FUNCTIONS
- PREGNANCY ANEMIA
- DO AND DONT DURING PREGNANCY
- ERECTILE DYSFUNCTION
- U.T.I IN PREGNANCY
- STROKE RISK
- EAT THIS NOT THAT
- HOOKWORMS INFECTION
- OMEGA 3 BENEFITS
- FASTING
- WEIGHT LOSS TIPS
- vitiligo
- ABORTION
- DENGUE VIRUS
- EBORA VIRUS
- FEVER
- URINARY TRACT INFECTION
- HOSPITAL INFECTIONS
- WEST NILE VIRUS
- YELLOW FEVER
- EYE DISEASE
- ZIKA VIRUS
- STRESS
- IRON DEFFICIENCE
- INSOMNIA (SLEEPING PROBLEMS)
- HEART PROBLEMS
- COMPONENTS OF BLOOD
- BLOOD DISORDER
- LABORATORY TEST OF BLOOD DISORDER
- BONE MARROW EXAMINATION
- BLOOD ANEMIA
- ANIMAL BITES
- EYE BURN
- CHOCKING
- HEAT STROKE
- SMOKE EFFECTS
- SNAKE BITE
- MALARIA VACCINE
- BEST WAY TO SLEEP A CHILD
- CHILD FEVER REDUCING
- ELEPHANTIASIS
- WOMEN BEARDS
- DATES
- PAPAYA FRUITS









0 Comments