Common Cold
(Upper Respiratory Infection; URI; Coryza)
The common cold is an acute, usually afebrile, self-limited
viral infection causing upper respiratory symptoms, such as rhinorrhea, cough,
and sore throat. Diagnosis is clinical. Handwashing helps prevent its spread.
Treatment is supportive.
About 50% of all colds are caused by one of the > 100
serotypes of rhinoviruses. Coronaviruses cause some outbreaks, and infections
caused by influenza viruses, parainfluenza viruses, enteroviruses,
adenoviruses, respiratory syncytial viruses, and metapneumoviruses may also
manifest as the common cold, particularly in patients who are experiencing
reinfection.
Rhinovirus infections are most common during fall and spring
and are less common during winter.
Rhinoviruses are most efficiently spread by direct
person-to-person contact, although spread may also occur via large-particle
aerosols.
The most potent deterrent to infection is the presence of
specific neutralizing antibodies in the serum and secretions, induced by
previous exposure to the same or a closely related virus. Susceptibility to
colds is not affected by exposure to cold temperature, host health and
nutrition, or upper respiratory tract abnormalities (eg, enlarged tonsils or
adenoids).
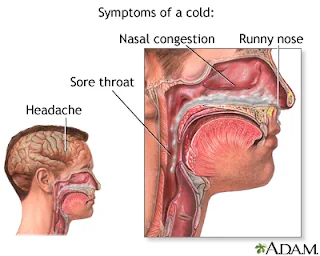
Symptoms and Signs of Common Cold
After an incubation period of 24 to 72 hours, cold symptoms
begin with a scratchy or sore throat, followed by sneezing, rhinorrhea, nasal
obstruction, and malaise. Temperature is usually normal, particularly when the
pathogen is a rhinovirus or coronavirus. Nasal secretions are watery and
profuse during the first days but then become more mucoid and purulent.
Mucopurulent secretions do not indicate a bacterial superinfection. Cough is
usually mild but often lasts into the 2nd week. Most symptoms due to
uncomplicated colds resolve within 10 days.
Colds may exacerbate asthma and chronic bronchitis.
Purulent sputum or significant lower respiratory tract
symptoms are unusual with rhinovirus infection. Purulent sinusitis and otitis
media may result from the viral infection itself or from secondary bacterial
infection.
Treatment of Common Cold
- Symptomatic treatment
- No specific treatment for the common cold exists.
- Antipyretics and analgesics may relieve fever and sore throat.
- Nasal decongestants may reduce nasal obstruction. Topical nasal decongestants are more effective than oral decongestants, but the use of topical drugs for > 3 to 5 days may result in rebound congestion.
Rhinorrhea may be relieved with 1st-generation
antihistamines (eg, chlorpheniramine) or intranasal ipratropium bromide (2
sprays of a 0.03% solution 2 or 3 times a day); however, these drugs offer
minimal benefit and should be used with caution in older patients, people with
benign prostatic hypertrophy, or angle-closure glaucoma. First-generation
antihistamines frequently cause sedation, but 2nd-generation (nonsedating)
antihistamines are ineffective for treating the common cold.
Antihistamines and decongestants are not recommended for
children < 4 years.
Zinc, echinacea, and vitamin C have all been evaluated as
common cold therapies, but none has been clearly shown to be beneficial.
Antibiotics should not be given unless there is clear
evidence of secondary bacterial infection. In patients with chronic lung
disease, antibiotics may be given with less restriction.
Prevention of Common Cold
There are no vaccines for the common cold.
Polyvalent bacterial vaccines, citrus fruits, vitamins,
ultraviolet light, glycol aerosols, and other folk remedies do not prevent the
common cold. Handwashing and use of surface disinfectant in a contaminated
environment may reduce spread of infection.
Key Points
a)
Many viruses can cause the common cold;
rhinoviruses cause about half of colds.
b)
Susceptibility to colds is not affected by
exposure to cold, host health and nutrition, or the presence of upper
respiratory tract abnormalities.
c)
Antihistamines may be used to relieve
rhinorrhea, but they offer minimal benefit and should be used with caution in
older patients and avoided in children < 4 years.
d)
Topical and oral decongestants relieve nasal
obstruction, but repeated use may cause rebound congestion.
e)
Many substances have been evaluated for
prevention and treatment, but none has clearly been shown to be beneficial.








0 Comments